Osteoporosis:
A Closer Look into The Silent Epidemic
Osteoporosis is a significant public health threat affecting an estimated 200 million individuals worldwide, and it's only projected to rise with an aging population. This bone disease often works silently, only revealing its destructive path when a fracture occurs. This article highlights the osteoporosis epidemic, its causes, risk factors, and preventative strategies.
Understanding Osteoporosis
Osteoporosis, meaning 'porous bone,' is a condition where bone density and quality are significantly reduced. It is a silent but deadly disease, often called a "silent epidemic" because it can progress undetected until a fracture occurs.- According to the International Osteoporosis Foundation, osteoporosis causes more than 8.9 million fractures annually worldwide.
- By 2050, the worldwide incidence of hip fracture in men is projected to increase by 310% and 240% in women, compared to rates in 1990.
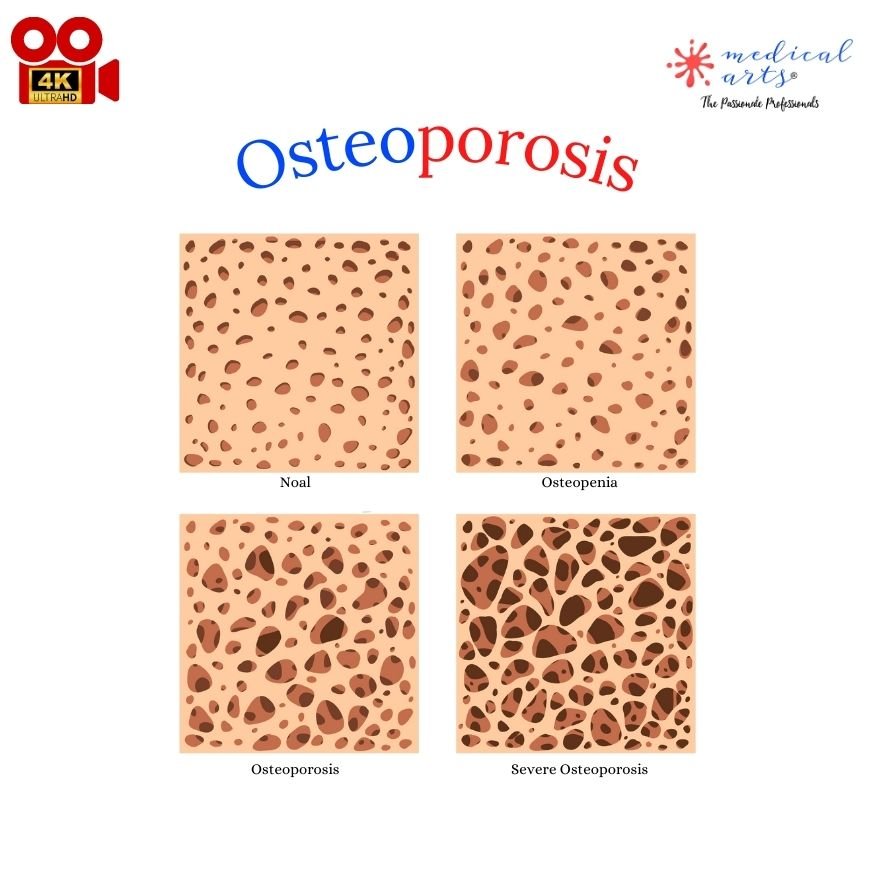
Osteoporosis and Osteopenia Pathophysiology:
The journey to osteoporosis often begins with osteopenia, a stage characterized by slightly lower-than-normal bone density. Understanding the pathophysiology—the functional changes accompanying this disease—offers crucial insight into prevention and treatment strategies.
The Bone Remodeling Cycle
Human bones aren't static structures but are constantly undergoing a process of breakdown (resorption) and rebuilding (formation). This bone remodelling cycle ensures healthy, strong bones and typically involves three main stages:-
Activation: Osteoclasts (cells that break down bone) move to the surface of the bone and start to dissolve the bone tissue, creating a small pit.
-
Resorption: The osteoclasts absorb the old bone tissue, which usually takes a few weeks.
-
Formation: After resorption, osteoblasts (cells that create new bone) fill the pit with new bone. This process takes several months.
The balance between bone resorption and formation is crucial. Any disruption to this equilibrium can lead to a loss of bone density.
Stage 1: Osteopenia
In the early stage of bone loss, known as osteopenia, bone resorption and formation balance begins to tilt. There is slightly more bone resorption than formation, leading to a mild decrease in bone density.- While not as severe as osteoporosis, individuals with osteopenia have a higher risk of progressing to osteoporosis if preventative measures aren't taken.
Stage 2: Osteoporosis
As bone loss continues, the individual eventually transitions into osteoporosis. Here, the rate of bone resorption significantly outweighs bone formation, leading to a substantial reduction in bone density.- At this point, the bones become porous, brittle, and more prone to fractures, even from minor falls or stresses.
Stage 3: Severe Osteoporosis
The same processes characterize severe osteoporosis as osteoporosis, but the loss of bone density is so great that fractures occur without any significant trauma or injury.- The most common fracture sites are the hip, spine, and wrist, but any bone in the body can be affected.
The progression from healthy bones to severe osteoporosis can take years or even decades, often without symptoms. This underscores the importance of regular bone density screening for early detection and timely intervention. Through lifestyle changes and medication, it's possible to slow down or even stop the progression of bone loss, reducing the risk of life-altering fractures.
Who's at Risk?
Osteoporosis can affect people of any age, but it is more common as people grow older, especially in post-menopausal women. This is due to the rapid decrease in estrogen levels, a hormone that protects against bone loss.- One in three women over 50 will experience osteoporotic fractures.
- One in five men aged 50 years and above are at risk of an osteoporotic fracture.
The Economic Impact of Osteoporosis
The financial burden of osteoporosis is massive and is projected to increase as the world's population ages.-
Osteoporosis costs the U.S. healthcare system an estimated $19 billion annually. By 2025, the costs could rise to as much as $25.3 billion annually.
-
In Europe, the economic burden of fragility fractures was estimated to be €37 billion in 2010; by 2025, it's expected to increase by 25%.
Prevention and Treatment
Several ways to prevent and manage osteoporosis include:
-
A balanced diet is rich in calcium and vitamin D.
-
Regular weight-bearing exercise.
-
Lifestyle changes like quitting smoking and reducing alcohol consumption.
-
Regular bone density testing is also crucial in early detection and prevention.
Optimal Nutrition for Bone Health
-
Calcium Intake: Calcium is the cornerstone of strong bones. Aim for a daily intake of 1000-1200mg for adults. Dietary sources include dairy products, green leafy vegetables, and calcium-fortified foods.
-
Vitamin D Consumption: Vitamin D assists in calcium absorption. Adults over 50 should strive for 800-1000 IU/day. Sunshine, fatty fish, egg yolks, and fortified foods are excellent sources.
-
Protein: Protein makes up about 50% of bone volume and around one-third of bone mass. Diets low in protein can lead to poor bone health and increase fracture risk. Good protein sources include lean meats, fish, dairy products, eggs, and plant-based sources like lentils, chickpeas, and nuts.
-
Magnesium: This mineral is essential for bone formation and influences the activity of osteoblasts and osteoclasts. Magnesium deficiency can lead to osteoporosis. Foods rich in magnesium include almonds, spinach, cashews, peanuts, and soya milk.
-
Vitamin K: Vitamin K2 plays a crucial role in bone mineralization. It works synergistically with vitamin D and calcium to keep your bones strong. Good sources of vitamin K include leafy green vegetables, broccoli, prunes, and fermented foods like natto.
-
Vitamin C: This is essential for collagen formation, a protein that is a significant part of bone tissue. Foods rich in vitamin C include citrus fruits, strawberries, bell peppers, and kiwi.
-
Zinc: This mineral helps stimulate the formation of bone-building cells and inhibits the resorption of bone. Zinc-rich foods include beef, shrimp, flax, oysters, and pumpkin seeds.
Weight-bearing and Muscle-strengthening Exercises
- Engage in weight-bearing exercises (like walking, jogging, or stair climbing) for 30 minutes on most days of the week.
- Strength training exercises, at least two days a week.
Osteoporosis Medication
Medication might be necessary when lifestyle changes and nutritional supplements aren't enough to stop bone loss or increase bone density.The choice of drugs depends on several factors, including the patient's age, gender, fracture risk, and whether they've had any fractures. Here are the primary categories of osteoporosis medications:
1. Bisphosphonates: This is the most common type of osteoporosis drug. They slow down the bone resorption rate, helping preserve bone mass and prevent fractures.
- Common bisphosphonates include alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast).
- Studies have shown that these medications can reduce the risk of fractures in the spine by up to 70% and in other parts of the body by up to 40%.
2. Hormone Replacement Therapy (HRT): This is often used to treat osteoporosis in women at menopause when estrogen levels fall dramatically.
- HRT can help maintain or increase bone density, thus reducing the risk of fractures.
- However, it is generally reserved for women with menopausal symptoms because long-term use of HRT can have some risks, including a slightly increased risk of certain types of cancer and cardiovascular diseases.
3. Selective Estrogen Receptor Modulators (SERMs): These drugs mimic the effect of estrogen on bone density in postmenopausal women.
- Raloxifene (Evista) is a commonly used SERM. It can reduce the risk of spinal fractures by about 30% in women with osteoporosis.
4. Parathyroid Hormone-Related Drugs: Medications like teriparatide (Forteo) and abaloparatide (Tymlos) mimic the hormone that regulates calcium levels in the body. They can stimulate new bone growth and reduce the risk of spinal fractures.
Regular use of these medications, combined with a lifestyle that promotes bone health, can significantly reduce the risk of fractures—an essential goal in the treatment of osteoporosis. Remember, each of these medications has benefits and risks, which need to be weighed individually. Always consult a healthcare provider for the most appropriate treatment strategy.
Regular medication use has been shown to reduce the risk of vertebral fractures by 40-70% and non-vertebral fractures by 20-50%.